Is Marburg Virus Disease (MVD) Outbreak Tip Of Iceberg? – Analysis
By Observer Research Foundation
By Viola Savy Dsouza, Jestina Rachel Kurian, Lada Leyens and Sanjay M Pattanhetty
The ongoing outbreak of Marburg virus disease (MVD) in Equatorial Guinea has once again highlighted the importance of public health approaches such as “One health” and the need for a collective effort to combat infectious diseases.
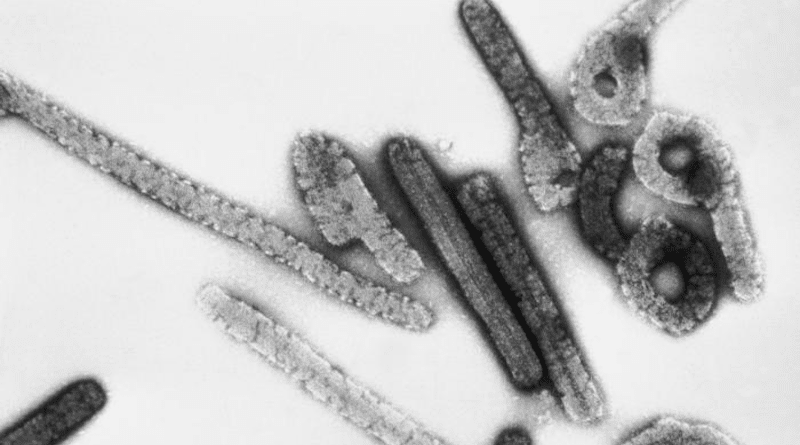
The MVD case fatality rate is around 50 percent which warrants global attention. In response to the outbreak, World Health Organization (WHO) R&D Blueprint organised an urgent meeting to set research priorities regarding the MVD outbreak. However, there is currently no specific treatment or vaccine for MVD despite sporadically re-occurring human fatality due to MVD reported since 1967 (Figure 1).
Additionally, the affected population reside within fragile health systems compounding the level of global health threat. For instance, a study on barriers to supportive care during the Ebola outbreak revealed lacunae in material and manpower, the deficit in the organisational structure of treatment units, and policy blind spots that impacted the effectiveness of responses. In order to strengthen the health system from threats such as Mpox and MVD, the global community has been negotiating a pandemic treaty as an international agreement for future pandemics.
The MVD outbreak has underscored the importance of a coordinated and collaborative response to emerging and re-emerging infectious disease threats. Scientists state that three out of four emerging infectious disease threats are zoonoses. To combat zoonotic diseases, measures such as Integrated Vector Management (IVM) model with evidence-informed decision-making, advocacy, capacity building, and collaboration as key elements that can be implemented to contain the outbreak.
For instance, a primary vector responsible for the transmission of the Marburg virus is the Rousettus Aegyptiacus bat. These bats are a reservoir for the virus and are known to transmit it to humans through close contact. IVM model can be used to target the vector population, i.e., by habitat isolation or using biological controls for population management.
Such measures can help to break the cycle of transmission between bats and humans. Similarly, an increase in evidence synthesis and research collaboration and maintenance of control measures are necessary to eliminate outbreaks and risks of resurgence. Integrating surveillance data to obtain a better understanding of the transmission dynamics of the Marburg virus will enable us to implement targeted interventions to reduce the risk of further spread.
It is also essential to amplify the voices of those who are most affected by such outbreaks, including healthcare workers, affected communities, and marginalised groups through community engagement and inter-sectoral coordination. For instance, the Ministry of Health (MoH) together with WHO, the US Centers for Disease Control and Prevention, and other international organisations have collaborated to initiate measures to control the outbreak and prevent further spread such as by supporting surveillance, community engagement, case management, laboratory services, contact tracing, infection control, logistical support and training and assistance with safe burial practices. Another effective way is addressing the structural inequalities that exist in our healthcare systems. This includes unequal access to healthcare, underfunding of public health programmes, and inadequate healthcare infrastructure.
Additionally, the MVD outbreak highlights the urgent need for a pandemic treaty to address global health threats. The pandemic treaty is an international agreement aimed at addressing global health threats by promoting greater collaboration and coordination among nations. It is an essential tool for addressing these challenges by ensuring that all countries have the necessary resources, tools, and expertise to respond effectively to future health emergencies.
This treaty would also create a framework for preparedness and response to future health emergencies, promote information sharing, and establish mechanisms for the equitable distribution of vaccines and other medical resources. The pandemic treaty can also help to amplify the voices of marginalized communities and those most affected by infectious disease outbreaks. By prioritizing their inclusion in the decision-making process, the treaty can ensure that the response efforts are targeted, effective, and equitable.
The COVID-19 pandemic revealed the tip of the iceberg, exposing the weakness in the pre-COVID health system. The pandemic treaty acknowledges that pandemics begin and end in communities and no one is safe till everyone is safe. While the zero draft of the pandemic treaty directs trials to be more coordinated and equitable in terms of access to resources, with rapid reporting and transparency as central to decision-making at all levels of governance, the treaty should include directives to conduct more fit-for-purpose trials and avoid research waste.
The continuing emergence and re-emergence of infectious diseases force us to recognise this is not the first nor the last infectious disease outbreak that we will face. Therefore, the time has come to set up a robust multilateral system for global health security that is inclusive, equitable, and fair. The question now remains—will the pandemic treaty adequately resolve the issues of the existing health system and prepare nations for a resilient future?