New Antiretroviral Drugs Decrease Chances Of HIV Sexual Transmission
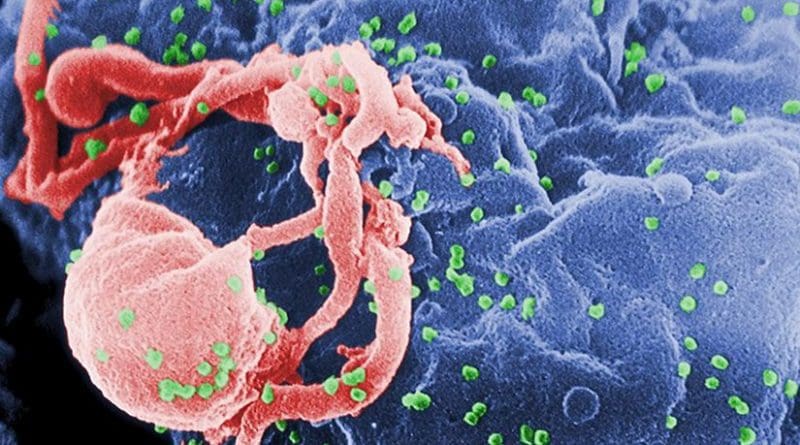
More than 2 million people got infected by human immunodeficiency virus (HIV) in 2015, being sexual transmission the main channel of infection. Researchers from the Infections of the Respiratory Tract and in Immunocompromised Patients group of the Bellvitge Biomedical Research Institute (IDIBELL), led by Dr. Daniel Podzamczer, have evaluated the speed at which a new antiretroviral drug, Dolutegravir, is able to reduce the viral load in semen, an area of the body considered to be a reservoir of the virus and where access for drugs is more difficult.
The results, published in Journal of Infectious Diseases, show the potential of these new treatments to reduce the chances of sexual transmission of the virus.
Current antiretroviral treatments are able to decrease blood viral load and make it undetectable in most patients within six to nine months of starting treatment, although it is estimated that about 5-25% of patients maintain detectable levels of virus in their semen after this time due to several factors, which are not always known.
“Therefore, in the case of serodiscordant couples, in which only one of the members is carrying the virus, in addition to condoms it is recommended that the seronegative person also takes antiretroviral drugs as prophylaxis while the viral load of their partner decreases in both blood and reservoirs”, sad Dr. Podzamczer.
However, there are new drugs, known as integrase inhibitors, which can act much faster.
“In this study we have focused on evaluating the rate of viral load drop in patients receiving these new treatments, namely Dolutegravir”, explained Dr. Arkaitz Imaz, first author of the study. “We have measured the viral load in blood and semen before starting treatment, at 3 days, at 7, at 14, at one month, at three months, and at six months. We know that viral load drop goes quick during the first few days/weeks, then slower and it finally stabilizes. Adapting a complex mathematical-statistical model to our data and to the characteristics of our patients, we have been able to obtain a kinetic model of the specific viral load drop for each compartment, blood and semen, with this treatment regimen”.
The researchers observed that while the rate at which viral load falls during the first few days is significantly higher in blood than in semen, it is equal during the second phase of fall. However, despite the speed difference, viral load becomes undetectable faster in semen than in blood because the base values are much higher in blood, ie there are many more viruses to eliminate.
“These results suggest the possibility of reducing the time of previous antiretroviral prophylaxis when using these new treatments,” the researchers noted.
On the other hand, the fall pattern is much more homogeneous in blood than in semen; This heterogeneity demonstrates the differential and more unpredictable nature of semen as a reservoir of the virus. In this sense, it is interesting to note that there is no clear correlation between the concentration of drug in semen and the decrease in viral load: “the concentration of dolutegravir in semen is more than enough to ensure viral load drop in this reservoir”, explained Dr. Podzamczer, “because even though only 7-8% of the drug in the blood reaches the semen, the proportion of active drug is much higher than what the observed in blood. This was something that we did not know until now “.
Integrase inhibitors are currently recommended by all clinical guidelines as the first line of treatment.
“Our study reinforces this decision, especially in light of the current HIV transmission landscape. If we reduce the time of viral load drop we clearly reduce the possibility of transmission, especially in groups at risk”, argued Dr. Imaz. In the editorial that Journal of Infectious Diseases dedicates to the article, it is pointed out the need to replicate this study with other new drugs currently under development, namely long-term antiretrovirals, to evaluate the potential of these new therapies and their activity in this viral reservoir.